By Harajana Umar Ragada
It all began with a small lump on her left breast. Over time, it grew larger with each passing day. Concerned, her husband took her to the hospital, where they were informed that a minor surgery was necessary. The doctor assured them of its safety and that she would go home immediately after the procedure.
However, an elderly woman approached her with a warning. She advised against allowing anyone to touch her breast at such a young age, claiming it was too risky. Unfortunately, she heeded the woman’s advice, ignoring her husband’s attempts to convince her otherwise. Instead, she returned home and relied on local herbs, hoping for a cure.
To her dismay, the condition worsened and developed into cancer. She underwent numerous treatments, including chemotherapy. I watched as she silently suffered, fervently praying for her quick recovery. However, she eventually succumbed to the illness after a lengthy stay at the hospital. She left behind three children, with the youngest just weaned off due to the mother’s illness.
Her death deeply affected me and shed light on the lack of awareness among many women about breast cancer, its preventive measures, predisposing factors, and signs to look out for.
According to findings from the World Health Organisation (WHO), in Nigeria alone, over 10,000 women die annually from cancer-related issues, with approximately 250,000 new cases recorded every year. These numbers are alarming, prompting me to contemplate how I could help.
That’s when I discovered Raise Foundation, an organisation dedicated to providing free cancer screening, raising awareness about breast cancer, and supporting patients through their journey, founded by the wife of the former Niger State Governor, Haj. Amina Abubakar Bello.
In an interaction with the CEO of Raise Foundation, Mrs Toyin Dauda, she disclosed that their mission is to create awareness and opportunities for women and girls, allowing them to realise their full potential in a safe environment for pregnancy and childbirth. They aim to empower women to make informed decisions and seize available opportunities.
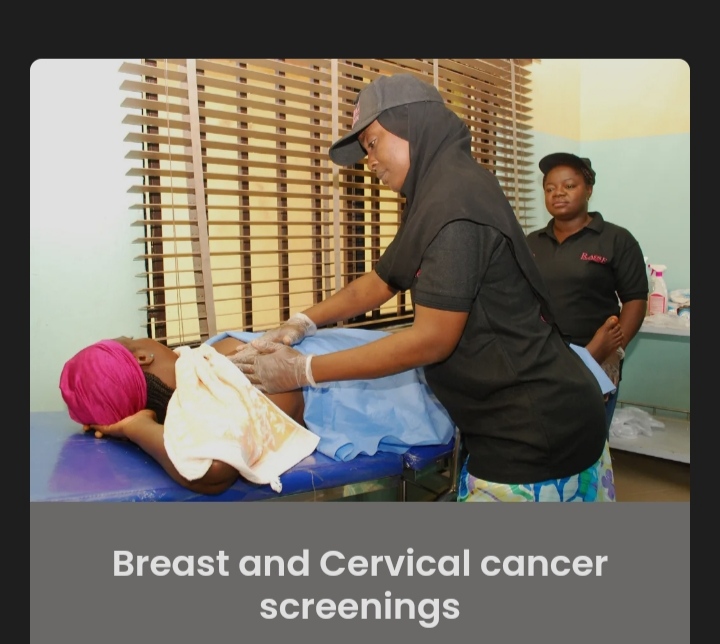
“We established the Raise Foundation in 2015, and we are proud to have the first breast and cervical cancer screening centre in Niger State. Additionally, we conduct outreach programs in hard-to-reach areas, where we screen women and educate them about breast cancer. We promote early detection and offer assistance to those diagnosed with cervical or breast cancer,” She affirmed.
Mrs.Toyin further explained that the screening is completely free of charge. Their healthcare professionals use gloves for examination, and if they identify any abnormalities or lumps, the woman will need to undergo a scan, which costs ₦4000. For women over 35, a mammography is recommended, priced at ₦10,000.
However, during October, Breast Cancer Awareness Month, they provide all these services for free. Operating from Monday to Friday, 9 a.m. to 4 p.m., Mrs Toyin urged women not to wait for the designated month but to seek screenings earlier. The foundation also guides self-breast exams.
Moreover, the Raise Foundation offers financial support for breast cancer patients. Rather than giving patients money directly, they cover the costs and provide receipts. They have partnerships that help fund their initiatives, allowing them to support women across Nigeria. Mrs Toyin appealed to governments, organisations, and individuals to contribute funds as the number of patients rose.
Furthermore, the program coordinator for Raise Foundation, Dr Fatima Tafida, emphasised the importance of understanding the risk factors associated with breast cancer and taking action to address them. She highlighted the risk factors, the consequences, the signs and symptoms, preventive measures, and how to perform self-breast exams.
According to Dr Fatima, the risk factors include being female, as breast tissue is present, an increasing trend of breast cancer among younger women (even as young as 25 years), early onset of menstruation, late menopause, not having been pregnant or breastfed, family history of breast cancer, smoking, excessive alcohol consumption, and poor diet or obesity.
She added that cancer is a significant threat as it impacts individuals socially, physically, emotionally, and financially.
“Signs and symptoms of cancer can vary depending on the type. The most common sign is the presence of a small lump in the breast, which may or may not be painful. Other indicators include the growth of the lump, cracks on the nipples, or the presence of bloody or Clear discharge. Unfortunately, many individuals are unaware that they have cancer until it has progressed.
“To prevent cancer, there are several measures that can be taken. Firstly, creating awareness about the disease and its risk factors is crucial. Secondly, modifying one’s lifestyle by quitting smoking and reducing alcohol consumption is essential. Additionally, individuals who are obese should aim to lose weight and incorporate regular exercise into their routine. Maintaining a balanced diet is also important in preventing cancer. Conducting regular self-breast exams is recommended for those with a family history of the disease. Lastly, performing self-breast exams at the end of the menstrual cycle can help in the early detection of any abnormalities.” She stressed.
Dr Fatima Tafida also underlined the importance of regular self-breast exams. She provided step-by-step instructions on how to perform a self-exam for early detection.
She advised standing in front of a mirror with the left hand raised above the head. Using the fingers of the right hand, one should palpate the whole breast, pressing the nipple and checking for any cracks or nipple discharge, be it bloody or clear. The person should then move their hand under the armpits and check for enlarged lymph nodes.
Dr. Fatima also highlighted signs to look out for, such as an orange peel appearance of the skin, one breast being bigger than the other, nipple retraction, or sores around the breast or nipples. These indicators could suggest a problem, and medical attention should be sought immediately.
She stressed the importance of early detection and shared the example of Angelina Jolie, who underwent a double mastectomy after testing positive for a breast cancer gene due to her family history.
For women over the age of 40, Dr. Fatima underscored the importance of getting a yearly mammogram. She advised against relying solely on herbal medicines and encouraged sticking to scientifically proven methods of treatment and prevention. She said teenagers should be aware and proactive in screening themselves. While adding that wearing bras made from secondhand clothes, often of European origin, does not increase any chance of having breast cancer.
In conclusion, Dr. Fatima appealed to society to show kindness and support to breast cancer patients. She highlighted the high costs associated with treating breast cancer and urged governments, NGOs, and individuals to provide assistance and support to these patients.
The Raise Foundation has received heartfelt gratitude from beneficiaries who have received free treatment and support. One patient expressed her appreciation, acknowledging that she would not have been able to afford the treatment without the foundation’s help. Another beneficiary thanked the foundation and called on the state government, NGOs, and individuals to support breast cancer patients.
As breast cancer continues to devastate lives, we must come together and fight it collectively. Let us join hands in raising awareness, providing support, and working towards a future where breast cancer no longer exists.
Harajana Umar Ragada wrote via kharajnah@gmail.com.