By Fadhila Nuruddeen Muhammad
The journey towards becoming a doctor often begins in childhood, driven by a deep desire to help others and positively impact people’s lives. For many, like myself, the path may take unexpected turns, leading to different callings. I recall my childhood fascination with medicine, even playfully emulating the role of a doctor in my school days, using improvised tools such as cloth face masks and hand gloves to “perform surgery” on classmates’ pens. I’d then transfer the ink from one tube to another, all to save my classmates from running out of ink. Life has a way of guiding us, and for me, that path led to journalism.
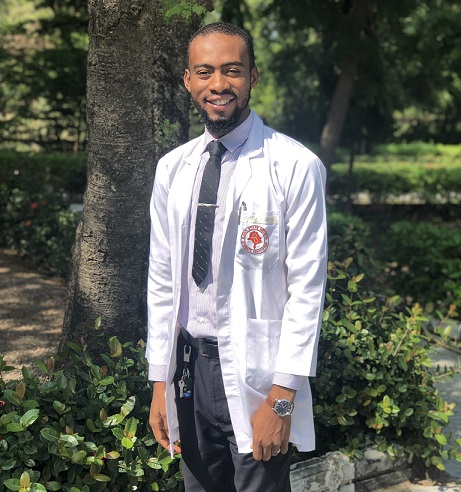
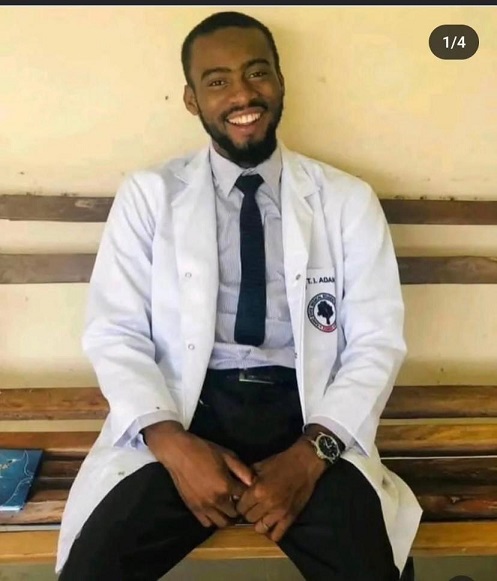
Tijjani Ibrahim, however, followed his childhood passion to become a committed and dedicated young medical doctor. His journey was filled with promise, but it took an unfortunate turn when he was diagnosed with advanced Chronic Liver Disease, Liver Cirrhosis, a consequence of Hepatitis B Viral Infection in June 2023.
Dr Aisha Danbatta, a medical consultant at Murtala Muhammad Specialist Hospital, explained Hepatitis B as a global health challenge that targets the liver, causing both acute and chronic illnesses. “This virus can be transmitted through various means, such as from mother to child, unscreened blood transfusions, exposure to contaminated materials, sexual contact with an infected partner, and even through saliva. Unlike HIV, Hepatitis B has a longer lifespan, making it easier to transmit.”
Dr Danbatta emphasised the prevalence of undiagnosed cases due to a lack of immunisation, leaving many unaware of their condition. Those diagnosed often struggle to afford vital tests like viral load measurements, which determine the quantity of the virus in the blood and assess the extent of liver damage. Physical examinations, ultrasounds, and fibroscans are also crucial in evaluating liver fibrosis and scarring monitoring the progression of the disease.
Dr Tijjani was first at the National Hospital, Abuja, where he was doing his house job and diagnosed with Liver Cirrhosis at the same hospital in June this year. The cost of his treatment was quite high, and he could not afford it. The National Hospital Abuja could only support his medical bills by creating an official memo. He was later transferred to Aminu Kano Teaching Hospital in Kano.
Hamza Danyaro, a friend of the late Dr Tijjani Ibrahim, explained that “his return to Kano was motivated by the hope that the National Medical Association (NMA) Kano State chapter could provide support. However, it was revealed that to benefit from their assistance, he needed to complete his National Youth Service Corps (NYSC), pay his dues, and work for at least a month or two before becoming eligible.”
“Tijjanii was not strong enough to go through these. Instead, we rallied to seek help from dignitaries such as politicians, the House of Representatives members of his local government in Kumbotso, and organisations. Unfortunately, the lengthy protocols inherent in today’s politics prevented direct outreach,” Danyaro added.
Tijjani was left with no other option than to seek funds. His friends organised the fundraising. The campaign was expected to raise a sense of urgency and necessity to help support a young medical doctor with funds to support his medical bills. This kind of transparency can prompt people to contribute to the cause. But only a tiny amount was raised after several days of campaigns.
Fauziyya D. Sulaiman, a philanthropist with a heart of gold, shared her disappointment on social media, writing, “It’s unfortunate that despite our community boasting politicians and business leaders among us, we couldn’t muster N25,000,000 to support Tijjani. If this were about some trivial matter, you would have seen some of us at the forefront. This is undeniably a disgrace.”
Dr Khalid Sunusi Kani, a medical doctor and health advocate, penned an open letter addressed to President Bola Ahmad Tinubu through Solacebase online newspaper. In this heartfelt letter, he expressed the critical need for Dr Tijjani Ibrahim’s services in Nigeria, emphasising the pressing issues within the country’s healthcare sector and the alarming rate of “brain drain syndrome.”
He wrote, “Your Excellency, Nigerians too are in desperate need of his services, looking at the manpower deficit in the health sector and the rate at which we suffer from ‘brain drain syndrome.’ I strongly believe Nigeria and Nigerians are unprepared and cannot afford to lose someone like Dr. Tijjani Ibrahim.”
Chronic Hepatitis B places individuals at a high risk of cirrhosis and liver cancer, leading to severe health consequences. In July 2023, the World Health Organization revealed that 296 million people were living with chronic hepatitis B infection in 2019, with 1.5 million new conditions occurring yearly. While there is no specific treatment for acute hepatitis B, medicines can effectively slow the progression of cirrhosis, reduce the incidence of liver cancer, and improve long-term survival.
Dr Tijjani Ibrahim died on September 6, 2023. His dedication to the medical field and his efforts to make a difference in the lives of others will be remembered and cherished.
Witnessing a doctor who devoted his life to saving countless others facing such challenging circumstances is genuinely disheartening. He dedicated his life to the mantra of ‘One Life, One Liver,’ yet our society struggled to come together to save his life. In a world where trivial issues on social media can garner an astonishing number of likes, it’s heartbreaking that Tijjani needed just 25,000 people to contribute a mere dollar each or someone who can just pay the total amount.
Tijjani’s story serves as a poignant reminder of the power of collective action and the importance of rallying together to support those in need, especially those who have dedicated their lives to serving others. Let us reflect on this unfortunate situation and take it as a call to action. Together, we can make a difference and ensure that the heroes who dedicate their lives to saving others do not suffer in silence.
“One Life, One Liver”: A heartfelt tribute to a fallen hero leaving an indelible mark on the world. May Allah rest his soul, amin.
Fadhila Nuruddeen Muhammad is a social media influencer based in Kano and can be reached via fadhilamuhd@gmail.com.