Dr. Ismail Muhammad Bello
Beyond hospital settings, harmful practices persist, particularly in developing countries where obtaining drugs over the counter is prevalent, and drug vendors may lack comprehensive knowledge of medications and diseases. From Penicillin to Ceftriaxone, these precious drugs, which require protection, can be obtained without prescriptions, posing a significant threat.
The ease of access to drugs has paved the way for self-treatment or “chemist” consultations, fostering malpractices. Again, a frequent occurrence is the prescription of antibiotics for the common cold. Research indicates that the common cold is predominantly caused by viruses, which are not responsive to antibiotics. It is a self-limiting condition that can be managed with measures such as steam inhalation, antihistamines like loratadine, and decongestants.
Similar to the common cold, most cases of sudden onset of watery stool, not stained with blood or mucus, with or without vomiting, are often of viral origin. This is typically a self-limiting condition that usually does not require antibiotics. In the management of diarrhoea, especially in children, the primary focus is on fluid therapy using Oral Rehydration Solution (ORS). Drug treatment is seldom beneficial, and antidiarrheal (antimotility) drugs can be harmful. Unfortunately, many individuals quickly resort to taking Flagyl, Loperamide, or Lomotil at the onset of diarrhoea.
However, bloody or mucoid stool, high fever, severe abdominal pain and prolonged diarrhoea are pointers to more serious conditions that may warrant antimicrobial use and should be quickly evaluated by a qualified doctor. In such instances, the use of antimotility agents is highly discouraged as it could lead to catastrophic outcomes like bowel perforation.
Another problem that continues to fuel this issue is the widespread and perplexing “Malaria-Typhoid diagnosis.” The lack of clinical skills needed to appropriately discern acute febrile illnesses coupled with excessive reliance on the outdated Widal test is driving an alarming prevalence of this peculiar diagnosis.
Most cases exhibit a sudden onset of high-grade intermittent fever with chills and rigours, particularly worsening in the evening. This is usually associated with generalized body weakness and pain, with no symptoms attributable to the gastrointestinal system (abdomen). In a region and time where malaria is quite prevalent, this most likely suggests a simple case of Uncomplicated Malaria that should be managed as such. Strangely in our setting such cases are quickly subjected to not only Malaria but also Widal (Typhoid) tests at the request of a healthcare worker or even on self-referral.
Numerous studies have consistently demonstrated that the Widal test lacks high specificity, particularly in endemic zones such as ours, where repeated exposure to the bacteria is prevalent. Cross-reactivity with various diseases, including Malaria—a frequent cause of fever in Nigeria—and challenges in interpretation further restrict its reliability as a diagnostic indicator.
It is therefore evident that the indiscriminate demand for the Widal test is causing the over-diagnosis of Typhoid fever, leading to the inappropriate use of antibiotics.
This practice has also led to the wrong notion of “chronic symptomatic typhoid” among gullible persons. Typhoid fever is not in the league of HIV & Hepatitis B. Infection in typhoid does not endure indefinitely but could recur, especially when the underlying risk factors like unsafe water and poor hygiene persist.
Chronic carriers do exist but are typically asymptomatic, holding more significance for public health due to their ongoing shedding of bacteria in their stool, a phenomenon reminiscent of the famous story of Typhoid Mary. Hence, statements like “Typhoid dina ne ya tashi” (I have a flare of a longstanding typhoid infection) and “Typhoid dina ne ya zama chronic” (I have a chronic typhoid infection) are grossly inaccurate.
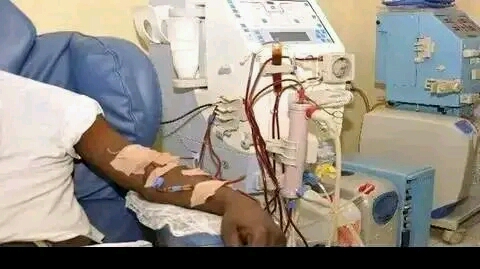
While not antibiotics, antimalarials, unfortunately, face their fair share of misuse. A prevalent mispractice involves the irrational use of injectable antimalarial drugs such as IM Arthemeter and even the almighty Artesunate. Nowadays, individuals often opt for injections, citing reasons like “I prefer not to swallow pills” or the perception of faster and more effective results. The most concerning scenario occurs when the condition is misdiagnosed as Malaria, especially in many “chemist” settings. This not only entails misuse but also results in economic waste, unnecessary stress, and the potential risks associated with injections.
Regrettably, injectable antimalarials are meant for treating severe forms of malaria, which someone walking into a chemist likely does not have. This is akin to deploying elite special forces for a minor crime. These forces should be mobilized only for significantly heightened threats or when the situation surpasses the capacity of initial responders.
Recommendations: The government plays a crucial role in this battle. Policies and regulations must be established to ensure the optimal utilization of these drugs. To address our persistent issue, these policies should not remain mere documents in offices but must be strictly enforced, with penalties imposed on those who violate them. These regulations should encompass various aspects, including the use of antibiotics in veterinary practice and food production, as well as proper oversight of the opening and operation of patent medicine stores.
Prevention is certainly better than cure. Tackling infectious diseases at the primary level is more impactful and cost-effective. The COVID-19 pandemic has underscored the significance of Water, Sanitation and Hygiene (WASH) in disease transmission & control. Hand hygiene, a practice widely adopted in 2020, stands out as the most crucial measure to prevent the spread of infections. Therefore it is crucial to provide communities with access to potable water and sufficient sanitary infrastructure to forestall the spread of these diseases in our society.
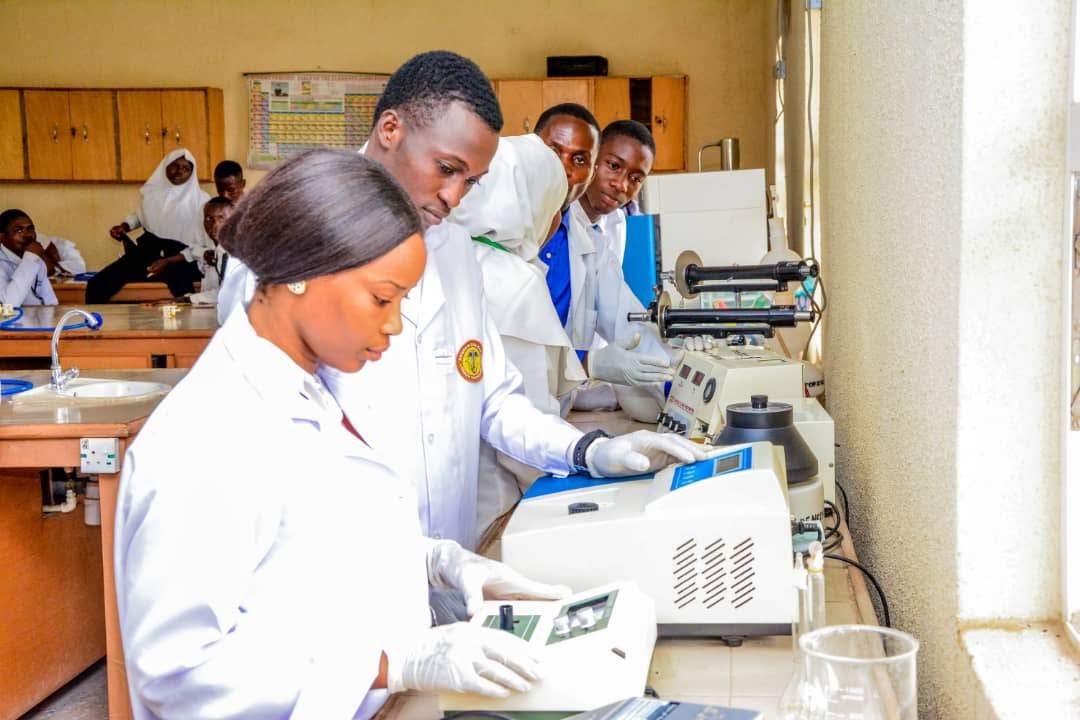
In managing most infections, a standardized treatment guideline outlines the specific drugs, their timing, and proper usage. You might be intrigued to discover that many practitioners may not even be aware of a specific Nigeria Standard Treatment Guideline document or other guidelines for various medical conditions.
In the absence of a local protocol, variations in management may arise among colleagues due to diverse backgrounds and training. Nowadays, particularly in secondary healthcare, many learn primarily through apprenticeship without referring to standards or understanding the rationale behind certain “innovative” practices. Unfortunately, what one is accustomed to may be incorrect and potentially harmful, or at best suitable only within the constraints commonly found at lower levels of healthcare.
Therefore, despite the challenges in our setting, doctors must prioritize continuous medical education to stay updated on global trends and standards while navigating the complexities of our setting. These innovations should not only be embraced as centre-specific practices or based on individual preferences like “this is how we do it in our centre” or “this is how Prof XYZ does it,” but they should also serve as opportunities for research and scientific validation.
Also, hospitals should formulate treatment protocols tailored to their unique circumstances, disseminate them widely, offer them as job aids at points of care, and ensure strict adherence by practitioners.
Furthermore, healthcare practitioners should dedicate time to counsel patients about the significance and potential risks associated with adhering to the prescribed dosage and duration of treatment. In well-established hospitals, it is imperative to institutionalize antimicrobial stewardship to ensure effective utilisation and surveillance of resistance patterns.
Ultimately, this is a battle declared by the microbial world on humanity, and everyone has a crucial role to play. Individuals should actively seek sound medical advice regarding diseases and treatments, avoiding the inclination to resort to self-help or patronize quacks. So when you take antibiotics for a simple common cold, know that you may be endangering humanity. When you fail to complete your antibiotics for the duration prescribed, you are surely endangering humanity. When you continue to treat typhoid when it is not the culprit, you are harming the patient and the world at large. Even you the medical practitioner, if you prescribe inappropriately, you are hurting the system.
Lastly, I encourage everyone to be advocates for responsible antibiotic use. Let’s utilize these valuable and endangered assets judiciously to avert a future where no drugs can cure pneumonia, syphilis, or meningitis – a potential regression to the 19th century. Remember, this is natural selection in action – it is not a lost battle but a fight for survival, one that we must undoubtedly triumph in. Dr. Ismail Muhammad Bello is a proud graduate of ABU Zaria. He is a Malnutrition Inpatient Care trainer and currently serves as a Medical Officer at both Khalifa Sheikh Isyaka Rabiu Paediatric Hospital in Kano and Yobe State Specialists Hospital in Damaturu. He can be reached at ismobello@gmail.com